Genetics maps end of the road for diabetes
Type 2 diabetes is a life-altering disease. And it’s known to cause 30 per cent of Canada’s strokes and 40 per cent of the country’s heart attacks.
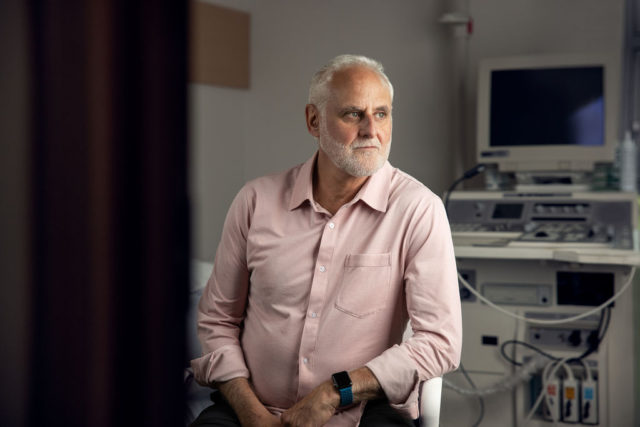
Can it be cured? Not yet. But every day, Dr. Robert Hegele works with patients to improve outcomes, reduce risks and discover the disease before it takes hold.
As one of the world’s leading authorities on cholesterol, Hegele routinely advises patients on how they can live longer and reduce their risk of serious health issues. Among the more than 2,500 patients in his care, he has noticed that when a patient has diabetes and high cholesterol, a hazard warning starts flashing on their risk of suffering a stroke or heart attack.
The good news, he says, is that it’s entirely within their power to fight the risk.
In the lab, Hegele targets one tiny molecule at a time and moves one step closer to preventing the onset of diabetes.
“We used to have this idea that there’s one gene responsible for diabetes, but it’s not quite that simple,” says Hegele, an internationally renowned endocrinologist and the medical director of the London Regional Genomics Centre. It’s at the Centre where his team studies the variants in the genetic code that can cause diabetes and cholesterol disorders.
A pioneer in developing diabetes medications, Hegele has used innovative treatments and game-changing technologies for patients with Type 2 diabetes at London Health Sciences Centre throughout the course of his award-winning career.
Using a diagnostic DNA panel that his lab invented, Hegele has discovered causal genes and mutations for more than 20 named medical conditions, including several inherited forms of diabetes.
His lab has shown that, in some cases, a single misprint in the DNA barcode is all that it takes to explain why a patient has diabetes. In most other cases, diabetes occurs because of the concerted effects of many genetic variants scattered throughout the patient’s genome.
He believes these human genome mapping efforts will provide even better understanding to why some people either can’t produce insulin or can’t properly use the insulin their bodies produce. Future advancements, Hegele says, will include better definition of diabetes subtypes, discovering targeted new treatments and even gene editing.
No matter what he finds, Hegele acknowledges for many patients with a genetic predisposition to Type 2 diabetes, environmental and lifestyle factors can contribute ultimately contribute to developing the disease. Many patients with diabetes also become susceptible to high cholesterol, which triggers the growth of fatty deposits in blood vessels. That in turn makes it difficult for blood to flow through arteries or – worse – the fatty deposits can break suddenly and form a clot, possibly causing a heart attack or stroke.
“In a patient with diabetes, treating cholesterol is almost as important as treating blood sugar. The complications we’re trying to prevent are things like amputations, strokes and heart attacks. We need to multi-task when managing genetic cardiovascular risk in patients with diabetes,” explains Hegele, a distinguished professor of medicine and biochemistry at the Schulich School of Medicine & Dentistry.
Preventing Type 2 diabetes, and one day eradicating it, is a complicated game. But Hegele, the world-class Western researcher with a singular focus on the miniscule, is making all of the right moves.