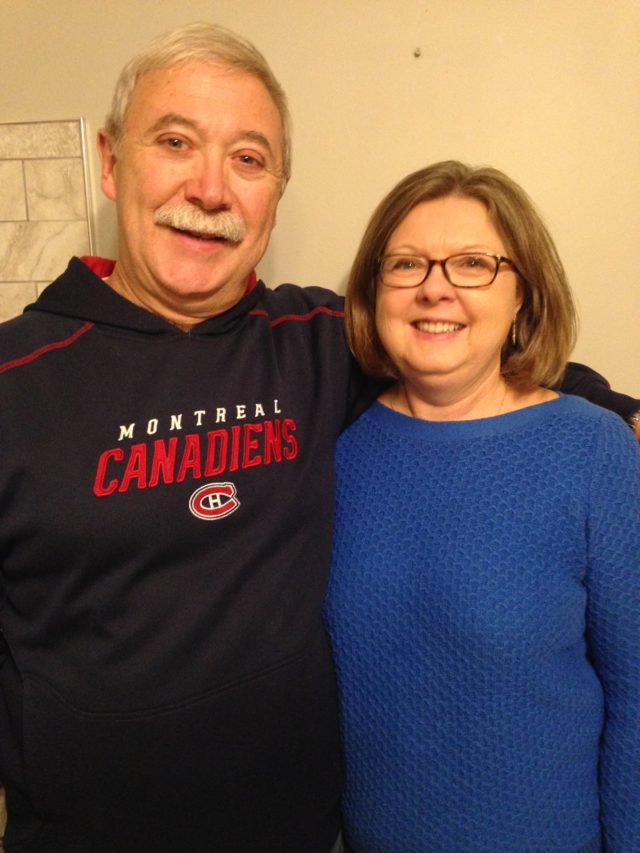
Fatigue, a lack of appetite, a racing heart, and rapid breathing are confusing symptoms for an 11-month-old infant and her parents. It took a trip to the Children’s Hospital Emergency Department and many tests before Michael Ketelaars and Tonya Gil’s daughter Brienne was diagnosed with Type 1 diabetes.
“We didn’t understand the diagnosis, or how it would change our life. We had never heard of anyone so young getting diabetes and didn’t realize that she would not grow out of it,” says Gil.
Following the midnight Emergency Department diagnosis, Brienne was then admitted to the Paediatric Intensive Care Unit with diabetic ketoacidosis, a serious complication of diabetes that develops when your body can’t produce enough insulin. “The shock during those next 12 hours was incredible. We experienced a large range of emotions and felt helpless. It took some time to realize she will be on insulin for the rest of her life,” adds Ketelaars.
Over the course of the next week, the health care team’s priority was stabilizing Brienne and teaching her parents how to care for an infant with diabetes. “The team wrapped their arms around us. Right away we entered two days of training as part of the Children’s Diabetes Clinic within the Paediatric Medical Day Unit. We started with the basics about diabetes, what to feed her, and when and how to dilute and administer insulin,” explains Gil.
As part of their training they received a backpack with educational materials. Included was a monkey named Coco. The parents used Coco as an education tool to explain to Claire, Brienne’s four-year-old sister, what was happening to Brienne. “Claire would come and give the monkey insulin. It provided a little bit of joy and reduced our stress,” says Gil, while laughing. “When we had to inject Brienne with insulin we would clap and say ‘yay,’ and she would also clap and say ‘yay’.”
After a month of treatment, Brienne’s weight gain was incredible. “We didn’t notice how small she was, even with regular measurement and family doctor appointments,” says Ketelaars. After three months, Brienne moved from pokes and needles to a continuous glucose monitor and insulin pump. Her parents can monitor her blood sugar levels instantly, even when she is sleeping.
“Brienne lacks the ability to communicate when she is feeling low. Technology allows her parents to see her blood sugar level every five minutes and always keep one step ahead of her body,” explained Shannon Hogeterp, registered nurse and diabetes educator at Children’s Hospital. “It is lifesaving.”
Now two years old, her parents describe her as a joyful child who is starting to find her language and discovering her personality. She celebrated her second birthday with a family barbeque and ice cream cake; her parents now knowledgeable enough to adjust her insulin to plan for the treats other children may take for granted.
Brienne returns to Children’s Hospital for a Diabetes Clinic check-in every three months. With their care team they discuss her progress and make little tweaks.
“In between our check-ins, we can upload information any time. Our care team will also ask for the information and we rely on their knowledge,” says Gil. Brienne will continue receiving care at Children’s Hospital until she is 18 when she will transition as an adult patient.
“Paediatric diabetes care is very different from adult care. Families consistently upload their children’s information and we are in touch often. We can quickly respond to highs, lows, and changes that happen as part of their life, like going to school,” explains Hogeterp.
As for the future, Ketelaars, who works with digital technology in mobile banking, says he has complete confidence that insulin administration technology will continue to evolve, maybe into a fake pancreas, or perhaps there will eventually be a cure for diabetes.
Until then, Ketelaars and Gil remain proud of their tough and resilient daughter.